Caretakers, educators, doctors, students, and people with diabetes themselves are often curious about national diabetes statistics. So, we took a look at some of your common questions and provided the figures to answer each of them. We hope this will help you to better understand diabetes and its associated risks, costs, and treatments.
How many Americans have Type 1 and 2 diabetes?
- As of 2014, an estimated 422 million people worldwide are estimated to have diabetes. (Word Health Organization)
- An estimated 23.1 million people in the U.S. have been diagnosed with diabetes. That’s an average of 7.2% of the U.S. population. (CDC, 2017)
- An additional 7.2 million people in the United States are estimated to have undiagnosed diabetes, making the total estimated sum of diabetic Americans 30.3 million. (CDC, 2017)
- An additional 2.9% of Americans are estimated to have undiagnosed diabetes. (CDC, 2017)
- 5% of diabetics are diagnosed with Type 1 diabetes; the rest have Type 2 diabetes. (CDC, 2017)
What is the prevelance of diabetes based on demographic details like age and race/ethnicity?
- 193,000 children and adolescents under 20 years of age (0.18% of the U.S. population) have been diagnosed with diabetes (CDC, 2017)
- 89% of people with diabetes are aged 45 and older. (CDC, 2017)
- Prevelance is significantly higher among American Indians/Alaska Natives (an estimated 14.9% of males and 15.3% of females have diabetes in this demographic). (CDC, 2013)
- Prevenance is also higher amongst Hispanic (12.6% males; 11.7% females) and non-Hispanic blacks (12.2% males, 13.2% females). (CDC, 2013)
- Prevelance is lower amongst Asian Americans (9.0% of males and 7.3% of females) and non-Hispanic whites (8.1% of males and 6.8% of females). (CDC, 2013)
- 12.6% of adults with less than a high school education have diagnosed diabetes, compared to 7.2% of those with most than a high school education. Of those who graduated high school, 9.5% have a diabetes diagnosis. (CDC, 2017)
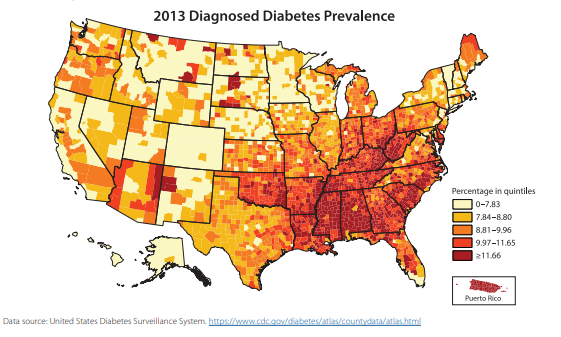
The above figures and heat map are from the Center for Disease Control (CDC) National Diabetes Statistics Report, 2017.
How common is prediabetes?
Prediabetes is determined based on a person’s fasting glucose or A1C level. When these levels are too high, a person is diagnosed with prediabetes.
- An estimated 33.9% of U.S. adults 18 and older have prediabetes (CDC, 2015).
- However, only 11.6% have been told by a health care professional that they have this condition, making it commonly undiagnosed. (CDC, 2015)
What are the reasons people diabetes are hospitalized? How often do hospitalizations occur?
- The yearly total of hospital discharges for diabetes-related illnesses is 7.2 million. (CDC, 2014)
- The yearly total of emergency department visits for diabetes-related complications is 14.2 million. (CDC, 2014)
- The leading causes of these discharges are major cardiovascular disease (1.5 million), lower extremity amputation (108,000), and diabetic ketoacidosis (168,000). (CDC, 2017)
- Note: to prevent foot or leg amuptation, it is recommended that people with diabetes take advantage of Medicare’s diabetic shoe coverage. Click here to learn more.
- An estimated 36.5% of U.S. adults with diagnosed diabetes have a crude prevelance of kidney disease. (CDC, 2017)
How common is diabetic neuropathy and other foot-related issues?
- An estimated 30 million Americans have some form of peripheral neuropathy. (Foundation for PN)
- Between 60%-70% of Americans with peripheral neuropathy (18-21 million) have diabetic neuropathy. (Foundation for PN)
- Acout 60-70% of people with diabetes have some form of diabetic nerve damage. (California Podiatric Medical Association)
- During their lifetime, 15% of people with diabetes will experience a foot ulcer. Of this group, 14-24% will require amputation. (California Podiatric Medical Association)
- Each year, more than 82,000 amputions are performed among people with diabetes. (California Podiatric Medical Association)
How much does diabetes cost Americans each year?
- The total direct and indirect cost of diagnosed diabetes in the U.S. is estimated as $347 billion as of 2017. This includes $237 billion in direct medical costs and $90 billion in reduced productivity. (ADA, 2018)
- The cost of diagnosed diabetes treatment has increased 26% over a 5-year period, from $245 billion in 2012 to the current $347 billion figure. (ADA, 2018)
- Hospital inpatient care makes up 30% of these costs, while prescription medications are another 30%. (ADA, 2018)
- The average annual medical expenditures for a person with diabetes is $16,752. Of that, an estimated $9,601 is used towards diabetes-related expenses. (ADA, 2018)
- Medical expenditures for those with diabetes are approximately 2.3x higher than they would be without diabetes. (ADA, 2018)
- In the U.S., 66% of costs related to diabetes are provided by government insurance (ie. Medicare, Medicaid, the military). (ADA, 2018)To see a list of all diabetic support products and services covered by Medicare, click here.
To order diabetic shoes covered by Medicare, click here.
Sources:
Center for Disease Control (CDC). National Diabetes Statistics Report. 2017.
American Diabetes Association. Economic Costs of Diabetes in the U.S. in 2017. Published by Diabetes Care, March 2018.
Mathers CD LoncarD. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med, 2006. 3(11):e442 – statistic republished via World Health Organization
California Podiatric Medical Association, Facts of Diabetes and the Foot, accessed Oct. 2018.



 TENS therapy uses small electrical impulses to block pain signals and increase endorphins. It is recommended by many pain management professionals as a non-invasive, non-painful and non-surgical way to treat neuropathy and similar conditions.
TENS therapy uses small electrical impulses to block pain signals and increase endorphins. It is recommended by many pain management professionals as a non-invasive, non-painful and non-surgical way to treat neuropathy and similar conditions. If you are feeling chronic pain in your feet, ankles, legs or even hips, there is some relief available: Medicare covers one pair of therapeutic shoes and three pairs of inserts for qualifying people each year. Even if the pain has not reached your feet, diabetic shoes can play an important role in protecting from future damage.
If you are feeling chronic pain in your feet, ankles, legs or even hips, there is some relief available: Medicare covers one pair of therapeutic shoes and three pairs of inserts for qualifying people each year. Even if the pain has not reached your feet, diabetic shoes can play an important role in protecting from future damage. Braces are commonly recommended by doctors and physiotherapists to reduce pain from free-moving joints. There are specific types of braces that may be more beneficial for long-term use by someone with chronic pain; for example, this product from
Braces are commonly recommended by doctors and physiotherapists to reduce pain from free-moving joints. There are specific types of braces that may be more beneficial for long-term use by someone with chronic pain; for example, this product from 

 In this study, “inactivity” was defined as less than 1,000 steps per day. This reflects the activity level of a person classified as “homebound”.
In this study, “inactivity” was defined as less than 1,000 steps per day. This reflects the activity level of a person classified as “homebound”. 


 Academy of Physician’s Assistants’ Board of Directors
Academy of Physician’s Assistants’ Board of Directors